Spirometry Machines
Spirometry Machines
A spirometry machine is a type of respiratory product used by medical professionals to monitor a patient's breathing. Our spirometry machines have been designed to make it easy for nurses to monitor patients with our range of innovative machines.
Whether you’re looking for a PC Based Spirometer or hand-held spirometer, Numed Healthcare offers the complete package for your GP surgery or clinic. We supply and support a range of desktop and PC based spirometry from leading brands, such as CareFusion (Micro Medical), NDD and Medchip.
Spirometry Machines for GP Surgeries or Health Centres
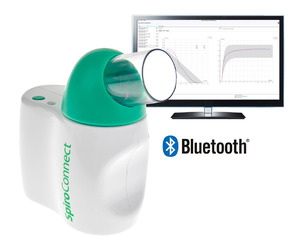
Designed for everyday use within the GP surgery or health centre, many of our spirometers are fully integrated with the Optum (EMIS), TPP SystmOne and Vision NHS GP clinical systems. One of our best-selling spirometers is the SpiroConnect spirometer. SpiroConnect is one of the most accurate and easy-to-use spirometers on the market.
FAQs
What is a spirometer machine used for?
A spirometer is a medical device used to perform breathing tests on patients with respiratory symptoms. It is used to diagnose, assess the severity, and monitor the progression of a variety of respiratory diseases.
What does a spirometer measure?
A spirometer measures:
Relaxed (or slow) Vital Capacity (VC) - The volume of air that can be slowly expelled from the lungs from a point of maximal inspiration to maximum expiration.
Forced Vital Capacity (FVC) - The volume of air that can be forcibly expelled from the lungs from a point of maximal inspiration to maximum expiration.
Forced Expiratory Volume in 1 second (FEV1) - The volume of air that can be forcibly expelled from the lungs from a point of maximum inspiration in the first second of an FVC manoeuvre.
FEV1/FVC ratio or FEV1% - The FEV1/FVC ratio is the FEV1 expressed as a percentage of the FVC (or VC if this is greater).
How do I quality control check my SpiroConnect?
Considering spirometry tests are used to measure lung function and diagnose potential respiratory conditions, accuracy is key. SpiroConnect has the very latest vertical turbine transducer to measure flows and volumes. This means that the calibration of SpiroConnect will not drift from its factory setting and you can be assured of accurate measurements. However, to conform to the current European guidelines for spirometry testing, the calibration of all spirometers should be regularly verified with a 3 litre calibration syringe. Read our guide on SpiroConnect calibration verification.
How is a spirometry test performed?
- Record the patient’s height, age and weight
- Ensure the patient is sat down comfortably and explain the procedure.
- Ensure the patient has a good seal around the mouthpiece. Advise them not to obstruct the mouthpiece with their teeth or tongue when blowing.
- Ask the patient to exhale fully and discourage them from leaning forward
- Perform VC and FVC. A minimum of three acceptable blows should be performed for each manoeuvre.
- Record the results.
You can read in more detail on how to perform a spirometry test here.
How do you clean a spirometer?
Hygiene is key with a spirometer. At Numed, we would recommend that after each patient, any consumables such as filters, mouthpieces and nose clips, are disposed of. Wipe down all parts that the patient has touched with a disinfectant wipe (If the wipe is wet, ensure no liquid seeps through the battery casing). You should also wipe the inlet where any condensation sometimes builds up.
After a day of use, disinfect the Spirometer transducer (in the SpiroConnect, this is the removable turbine). We would advise using the PeraSafe cleaning solution for this. However, ensure the transducer is fully dry before its next use, and do not submerge the handheld part of the SpiroConnect into the PeraSafe, as this could damage the internal components. Only the removable transducer can be submerged in the PeraSafe cleaning solution.
How should a patient prepare for a spirometry test?
Before a spirometry test, patients should be asked to avoid:
- Smoking for at least 24 hours before the test
- Eating a large meal before the test
- Vigorous exercise before the test
- Wearing tight-fitting clothing
What equipment is required to perform spirometry?
You will need some or all of the equipment below to perform spirometry testing, depending on the type of tests you are wanting to perform. For more information please contact our sales team who will be able to advise you based on your requirements.
Spirometer - This must meet ISO standard 26782 and be calibrated according to local guidelines. Many of our spirometers are fully integrated with the EMIS, TPP SystmOne and Vision NHS GP clinical systems using our innovative i3 software.
One-way disposable mouthpieces and nose clips – you can view our range of mouthpieces here.
Bacterial and viral filters – these should be used by any patients who are at any risk of infection.
Accurate height measures – these should be calibrated according to manufacturer’s instructions. We offer a range of height measures, some of which are integrated with the leading GP clinical systems.
Short-acting bronchodilators - for reversibility testing and suitable means for delivery
(volumatic/nebuliser)
What are the common mistakes in spirometry testing?
Some of the most common mistakes found in spirometry testing include:
A poor seal around the mouthpiece – ensure that the patient’s lips are fully sealed around the mouthpiece so no air can escape.
Poor intake of breath – encourage the patient to take as deep a breath as possible before each blow.
Hesitation or false start – encourage the patient to breathe out without any pauses or hesitation.
Early termination of exhalation – this a ‘short blow’ which has not achieved the full FVC. Encourage patients to exhale until all the air in their lungs has been completely expelled.
Incorrect data entered into the spirometer prior to testing – this can be prevented by using our SpiroConnect spirometer, which eliminates manual entry of patient data by integrating with your GP clinical system.
To avoid many of these mistakes, it is vital that spirometry testing is undertaken by a healthcare professional who is trained and accredited. It is usually advised that anyone undertaking the test is also trained in interpreting the results to ensure meaningful information is produced.
When should you conduct spirometer calibration?
Modern spirometers, such as SpiroConnect, are very accurate and only need calibration if they are damaged. However, local guidelines may require that calibration is performed more frequently.
Association for Respiratory Technology and Physiology (ARTP) guidelines recommend that spirometry equipment calibration should be performed before each session or after every 10th patient, whichever comes first. For a device to be within calibration limits, it must read +/- 3% of true.
Why is SpiroConnect so well suited to spirometry testing during the COVID-19 pandemic?
SpiroConnect has Bluetooth connectivity and can be connected to a desktop, laptop or tablet computer through glass or one or more plastic safety screens, at a range of up to 20 metres. These unique features mean that full spirometry tests can be performed with the patient seated in isolation from the medical professional. This means spirometry clinics can deliver spirometry testing with high levels of safety.